Home

This is the website of Brian Derbyshire PhD. You can view my credentials and papers on www.researchgate.net.
The following software is available to download.
Acetabular Cup Wear Volume
This software calculates acetabular cup wear volume using measurements taken from a single,
antero-posterior radiograph. Unlike other calculation methods, the software takes into account a
number of variables: femoral head size, wear penetration, wear direction, radial clearance and
version. The effect of radial clearance is particularly important for penetrations of less than 1mm
(See Derbyshire B. “The estimation of acetabular cup wear volume from two-dimensional
measurements: a comprehensive analysis” (https://doi.org/10.1243/0954411981534060 ).
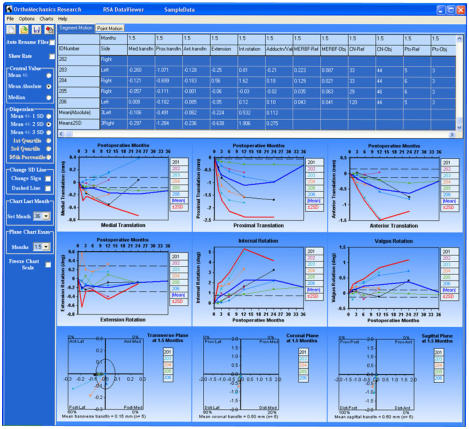
RSA DataViewer
This software is specifically for use in conjunction with UmRSA radiostereometric analysis software. UmRSA data files can be quickly selected and loaded into the DataViewer which immediately tabulates the data. Each data row corresponds to a time-series migration data set for each patient. Selection of a row or rows instantly plots the data on a series of commonly required charts. Data tables can be printed or exported to a spreadsheet. Charts can be exported for use in presentations/papers.
Acetabular Cup Orientation Measurement
This software can be used to measure acetabular cup orientation from a single antero-posterior
radiograph. Measurements from full-pelvis radiographs are corrected for X-ray beam offset. The
software is able to distinguish retroversion. Uncemented (metal shell) cups and resurfacing cups
can be measured. The software has been validated.
(DOI:https://doi.org/10.1016/j.arth.2013.06.024)

OrthoMechanics Research
RSA DataViewer
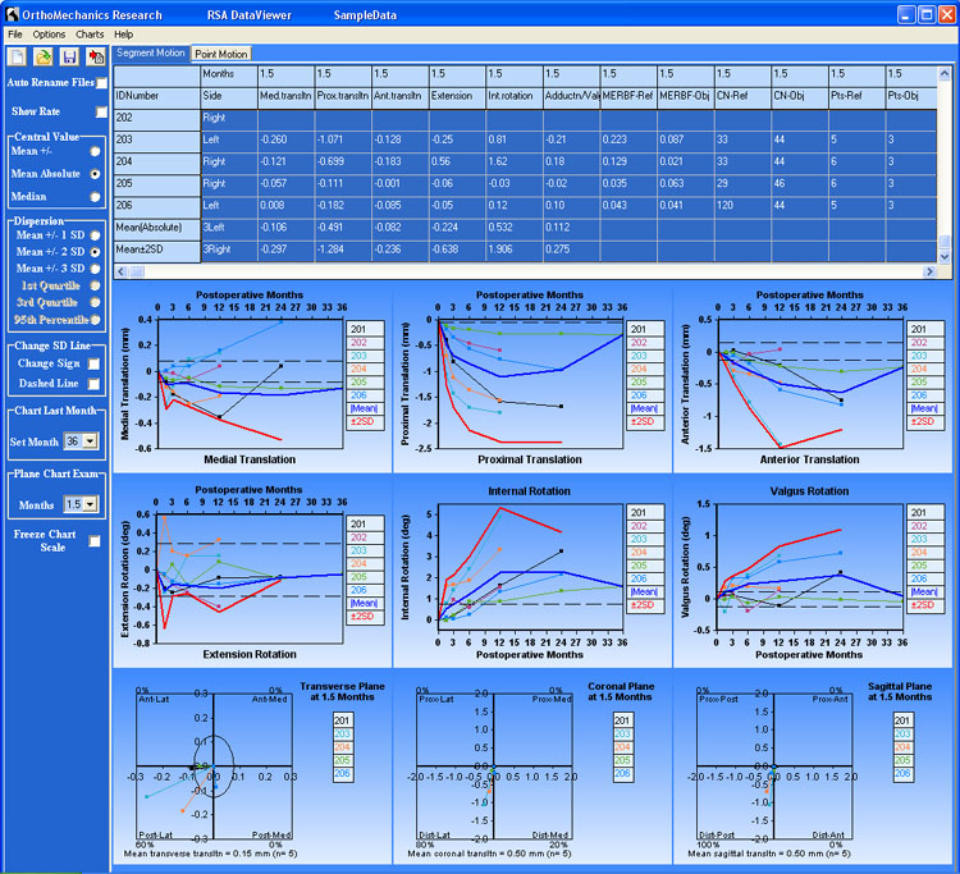
UmRSA produces a large amount of raw data from each measurement. Before the data can be analysed, it needs to
be organised according to the particular patient and RSA examination time, and the signs of some of the migration
components need to be changed according to the operation side of the patient. This normally involves a very
laborious and time -consuming process of manually transcribing the data to a spreadsheet and then creating charts
for each migration component. Errors can easily be introduced at this stage. RSA DataViewer solves all of these
problems. What could normally take hours can be accomplished in a matter of seconds.
Using RSA DataViewer
After each UmRSA measurement, the data is saved to a data file and you would normally save each file according
to the patient ID and examination time. However with RSA DataViewer, you don't even need to spend time writing
the patient ID and examination specific file names when saving the data files. Simply name each file, a, b, c ... etc
when saving the file in UmRSA, and RSA DataViewer will (optionally) re-name your data files (as it opens them)
according to the patient ID and the examination. RSA DataViewer then organises the migration results (including
condition number, Mean Error and number of points) into a scrollable table on two pages: a Segment Motion page,
and a Point Motion page. The signs of the data are automatically changed according to the operation side of the
patient. Each row of the table corresponds to a time-series, migration data set for each patient.
Select one or more of the table rows, and the migration graphs of the selected patients are instantly plotted in a
series of charts corresponding to each type of migration.
Key features of RSA DataViewer
•
plot graphs of migration or migration rate;
•
include graphs of mean and mean +/- SD (or median and median +/- quartiles);
•
show migration in the three planes: the % number of vectors in each quadrant indicates the variability of
migration direction within each plane;
•
name landmark points (e.g. shoulder, head, tip) for display in the Point Motion table and charts;
•
optionally include condition numbers or number of patients for each time point in each chart;
•
optionally include error bounds (determined from double examination measurements) on each chart;
•
copy and paste charts (enhanced metafile format) into a text document, spreadsheet or PowerPoint;
•
optionally remove chart title, chart colour, graph colours, legends, for black and white publications;
•
save the table for further analysis with statistics software;
•
Comprehensive Help File included.
Mouse Over the red rectangles for description of some of the features on the figure below:-








Calculation of Acetabular Cup Wear Volume
For many researchers in the field of total hip replacement, the depth of penetration of the femoral head into the acetabular
cup is considered to be the best way of reporting cup wear. This is a fallacy. The fundamental unit of wear is wear volume.
This is easily demonstrated by considering how, for a given wear penetration, an increased femoral head diameter would
produce more wear debris. In fact, several parameters are required to determine the wear volume: penetration, wear
direction, head diameter, socket diameter, and cup version angle.
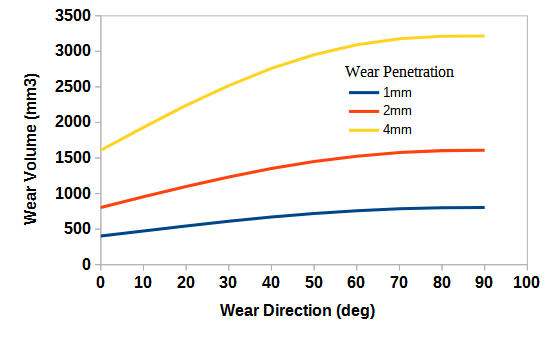
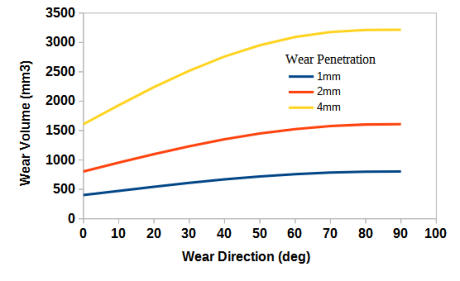
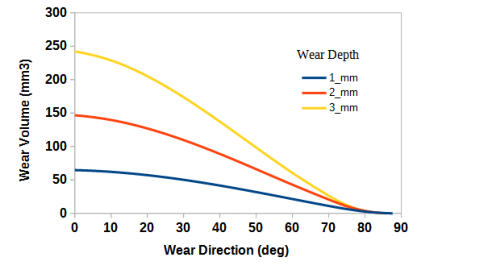
The chart on the left shows how the wear volume of
a purely hemispherical socket varies with wear
direction (relative to the base of the cup). The
volume doubles over the range 0 - 90
o
. In this case,
the initial diameter of the cup (32 mm) and the
diameter of the femoral head are the same (no radial
clearance).
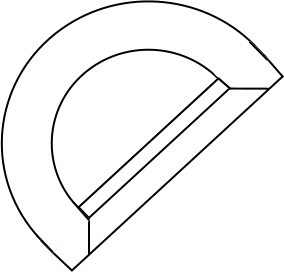
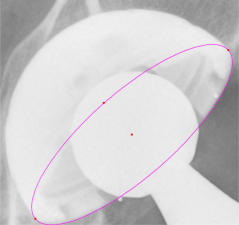
Due to manufacturing tolerance considerations, manufacturers always create small
difference in size betweem the femoral head and the cup socket. This ensures that the
head will always fit in the socket (radial clearance) at the time of operation. The
figure on the left shows a section through a plastic acetabular cup and a femoral head
component. The size difference (radial discrepancy) between the head an socket has
been exaggerated to show that early wear penetration doesn’t involve the whole
hemispherical section of the femoral head: only a button sized amount of the plastic
has been removed. It is not until the wear penetration exceeds more than 1mm that
the whole cross-section of the femoral head is involved in the wear process.
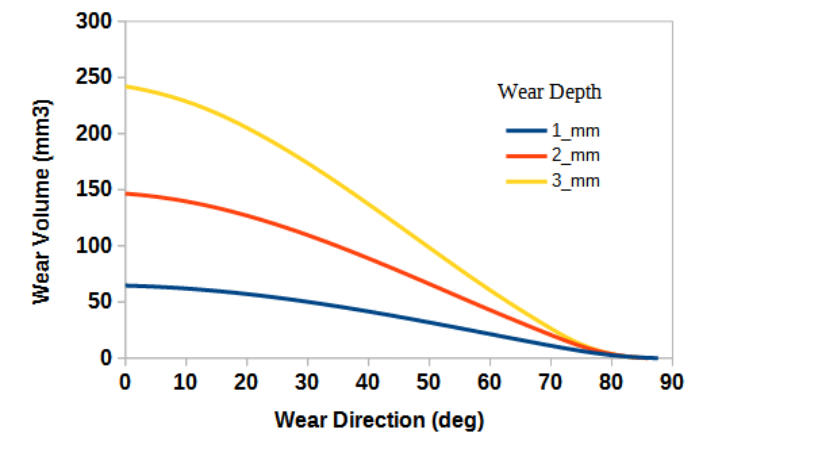
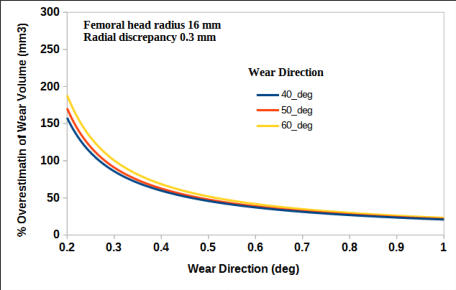
The figure on the left shows that,
at low wear depths, the wear
volume will be dramatically
overestimated if the effect of a
radial discrepancy is not taken
into account. These values have
assumed a creep penetration of
0.1 mm (assuming the same
amount of creep for fully
conforming and non-conforming
components) - so the calculated
volume is entirely due to wear.
In many cases, the cup socket comprises three shapes: hemisphere, cylindrical cut-out, and
conical chamfer (see figure). Depending on the wear direction, the wear depth and the
radial discrepancy, wear can involve all three of these elements. The volume of wear
debris can, therefore, be significantly more than that accounted for by wear of the
hemispherical portion alone.
The chart below shows the wear volume of the cylindrical and conical opening of a 32 mm
diameter head/cup (no radial discrepancy).


Acetabular Cup Orientation Measurement
Acetabular cup orientation is generally assessed visually from an antero-posterior
(AP) radiograph following implantation. For standard total hip replacements, it is
important that the inclination and anteversion are set within a certain range
1
(“safe
zone”) in order to avoid problems of impingement
2
with the femoral component
during all patient manoevres. For resurfacing hips, adverse tissue reactions and
high metal ion concentrations in the blood
3-5
have been associated with cup
orientations beyond a certain range.
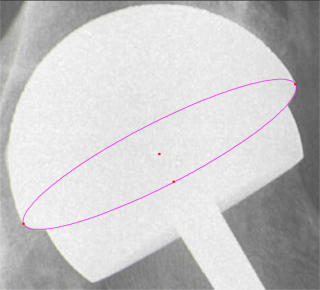
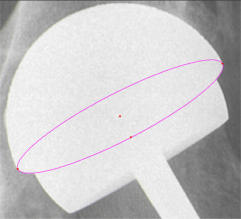
The measurement of “radiographic” version and inclination
6
from an antero-
posterior radiograph is carried out by measuring the geometry and orientation of
the projected ellipse of the cup opening. With uncemented cups, this is difficult
because the superior side of the metal shell opening is somewhat opaque and partly
obscured by the femoral head. With resurfacing cups, the situation is even worse:
only the extreme ends of the cup opening are visible on the radiograph. One way to
obviate this problem is to use image analysis software that can fit an ellipse to the
inferior half of the cup opening. The software, available here, automatically edge-
detects the visible lower region of the metal shell/cup, and regions of obscuration
can be avoided. The inclination (relative to a tangent line drawn between the
inferior borders of the ischial tuberosities) and the anteversion are automatically
calculated and tabulated. Both the inclination and anteversion are corrected for the
effect of X-ray beam offset
7
(i.e. when the beam is targetted in the region of the
pubic symphysis). The software has a facility to discern whether the cup is in
antversion or retroversion. This requires two AP radiographs: one standard pelvis
radiograph and one hip centred radiograph. These need to be taken in succession so
that the patient remains in the same position.
The software has been validated using radiographs of a laboratory model at
different settings.
8
1.
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip
replacement arthroplasties. J Bone Jt Surg Am. 1978;60:217-220.1.
2.
Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Jt Surg Am.
2007;89-A:1832-1842.
3.
Langton DJ, Jameson SS, Joyce TJ, Webb J, Nargol AVF. The effect of component size and
orientation on the concentration of metal ions after resurfacing arthroplasty of the hip. J Bone Jt Surg
Br. 2008;90-B:1143-1151.
4.
Hart AJ, Skinner JA, Henckel J, Sampson B, Gordon F. Insufficient acetabular version increases blood
metal ion levels after Metal-on-metal Hip Resurfacing. Clin Orthop Relat Res. 2011;469:2590-2597.
5.
Wynn Jones H, Macnair R, Wimhurst J, et al. Silent tissue pathology is common with a modern metal-
on-metal hip arthroplasty. Acta Orthop. 2011;82:301-307.
6.
Murray DW. The definition and measurement of acetabular orientation. J Bone Jt Surg Br. 1993;75-
B:228-232.
7.
Derbyshire B. Correction of acetabular cup orientation measurements for X-ray beam offset. Med Eng
Phys. 2008;30:1119-1126.
8.
Derbyshire B, Diggle PJ, Ingham CJ, Macnair R, Wimhurst J, Wynn Jones H. A new technique for
radiographic measurement of acetabular cup orientation. J Arthroplasty. 2014;29(2):369-372.

If you would like to receive software, or if you have any questions, please email:
briand@orthomech.co.uk
To download software, you will require a password for the download site.


Download CupOrientation Software Help File pdf
Download RSA DataViewer Software Help File pdf


Contact

Download Cup Orientation Software
Download Hip Wear Measurement Software





This is the website of Brian Derbyshire PhD.
You can view my credentials and papers on
www.researchgate.net.
The following software is available to download.
Acetabular Cup Wear Volume
This software calculates acetabular cup wear volume
using measurements taken from a single, antero-posterior
radiograph. Unlike other calculation methods, the
software takes into account a number
of variables: femoral head size, wear
penetration, wear direction, radial
clearance and version. The effect of
radial clearance is particularly
important for penetrations of less
than 1mm (See Derbyshire B. “The
estimation of acetabular cup wear
volume from two-dimensional
measurements: a comprehensive analysis”
(https://doi.org/10.1243/0954411981534060 ).
RSA DataViewer
This software is specifically for use in conjunction with UmRSA radiostereometric analysis software. UmRSA data files can be quickly selected and loaded into the DataViewer which immediately tabulates the data. Each data row corresponds to a time-series migration data set for each patient. Selection of a row or rows instantly plots the data on a series of commonly required charts. Data tables can be printed or exported to a spreadsheet. Charts can be exported for use in presentations/papers.
Acetabular Cup Orientation
Measurement
This software can be used to
measure acetabular cup
orientation from a single
antero-posterior radiograph.
Measurements from full-
pelvis radiographs are
corrected for X-ray beam
offset. The software is able to
distinguish retroversion.
Uncemented (metal shell)
cups and resurfacing cups can
be measured. The software
has been validated.
(DOI:https://doi.org/10.1016/j.arth.2013.06.024)

OrthoMechanics Research

If you would like to receive software, or if you
have any questions, please email:
Download CupOrientation Software Help File pdf
Download RSA DataViewer Software Help File pdf
briand@orthomech.co.uk
Please Note:
Software can only be downloaded onto a desktop computer


UmRSA produces a large amount of raw data
from each measurement. Before the data can be
analysed, it needs to be organised according to
the particular patient and RSA examination
time, and the signs of some of the migration
components need to be changed according to
the operation side of the patient. This normally
involves a very laborious and time -consuming
process of manually transcribing the data to a
spreadsheet and then creating charts for each
migration component. Errors can easily be
introduced at this stage. RSA DataViewer
solves all of these problems. What could
normally take hours can be accomplished in a
matter of seconds.
Using RSA DataViewer
After each UmRSA measurement, the data is
saved to a data file and you would normally
save each file according to the patient ID and
examination time. However with RSA
DataViewer, you don't even need to spend time
writing the patient ID and examination specific
file names when saving the data files. Simply
name each file, a, b, c ... etc when saving the
file in UmRSA, and RSA DataViewer will
(optionally) re-name your data files (as it opens
them) according to the patient ID and the
examination. RSA DataViewer then organises
the migration results (including condition
number, Mean Error and number of points) into
a scrollable table on two pages: a Segment
Motion page, and a Point Motion page. The
signs of the data are automatically changed
according to the operation side of the patient.
Each row of the table corresponds to a time-
series, migration data set for each patient.
Select one or more of the table rows, and the
migration graphs of the selected patients are
instantly plotted in a series of charts
corresponding to each type of migration.
Key features of RSA DataViewer
•
plot graphs of migration or migration rate;
•
include graphs of mean and mean +/- SD
(or median and median +/- quartiles);
•
show migration in the three planes: the %
number of vectors in each quadrant
indicates the variability of migration
direction within each plane;
•
name landmark points (e.g. shoulder, head,
tip) for display in the Point Motion table
and charts;
•
optionally include condition numbers or
number of patients for each time point in
each chart;
•
optionally include error bounds (determined
from double examination measurements) on
each chart;
•
copy and paste charts (enhanced metafile
format) into a text document, spreadsheet or
PowerPoint;
•
optionally remove chart title, chart colour,
graph colours, legends, for black and white
publications;
•
save the table for further analysis with
statistics software;
•
Comprehensive Help File included.
Calculation of Acetabular Cup
Wear Volume
For many researchers in the field of total hip
replacement, the depth of penetration of the
femoral head into the acetabular cup is
considered to be the best way of reporting cup
wear. This is a fallacy. The fundamental unit of
wear is wear volume. This is easily
demonstrated by considering how, for a given
wear penetration, an increased femoral head
diameter would produce more wear debris. In
fact, several parameters are required to
determine the wear volume: penetration, wear
direction, head diameter, socket diameter, and
cup version angle.
The chart above shows how the wear volume of
a purely hemispherical socket varies with wear
direction (relative to the base of the cup). The
volume doubles over the range 0 - 90
o
. In this
case, the initial diameter of the cup (32 mm)
and the diameter of the femoral head are the
same (no radial clearance).
Due to manufacturing tolerance considerations,
manufacturers always create small difference in
size betweem the femoral head and the cup
socket. This ensures that
the head will always fit
in the socket (radial
clearance) at the time of
operation. The figure on
the left shows a section
through a plastic
acetabular cup and a
femoral head
component. The size
difference (radial discrepancy) between the head
an socket has been exaggerated to show that
early wear penetration doesn’t involve the
whole hemispherical section of the femoral
head: only a button sized amount of the plastic
has been removed. It is not until the wear
penetration exceeds more than 1mm that the
whole cross-section of the femoral head is
involved in the wear process.
The figure below shows that, at low wear
depths, the wear volume will be dramatically
overestimated if the effect of a radial
discrepancy is not taken into account. These
values have assumed a creep penetration of 0.1
mm (assuming the same amount of creep for
fully conforming and non-conforming
components) - so the calculated volume is
entirely due to wear.
In many cases, the cup
socket comprises three
shapes: hemisphere,
cylindrical cut-out, and
conical chamfer (see
figure). Depending on the wear
direction, the wear depth and the
radial discrepancy, wear can involve
all
three of these elements. The volume of
wear debris can, therefore, be significantly more
than that accounted for by wear of the
hemispherical portion alone.
The chart below shows the wear volume of the
cylindrical and conical opening of a 32 mm
diameter head/cup (no radial discrepancy).

Acetabular Cup Orientation
Measurement
Acetabular cup
orientation is
generally assessed
visually from an
antero-posterior (AP)
radiograph following
implantation. For
standard total hip
replacements, it is
important that the
inclination and
anteversion are set
within a certain range
(1) (“safe zone”) in
order to avoid
problems of
impingement (2) with
the femoral
component during all
patient manoevres.
For resurfacing hips, adverse tissue reactions
and high metal ion concentrations in the blood
(3-5) have been associated with cup orientations
beyond a certain range.
The measurement of “radiographic” version and
inclination (6) from an antero-posterior
radiograph is carried out by measuring the
geometry and orientation of the projected ellipse
of the cup opening. With uncemented cups, this
is difficult because the superior side of the metal
shell opening is somewhat opaque and partly
obscured by the femoral head. With resurfacing
cups, the situation is even worse: only the
extreme ends of the cup opening are visible on
the radiograph. One way to obviate this problem
is to use image analysis software that can fit an
ellipse to the inferior half of the cup opening.
The software, available here, automatically
edge-detects the visible lower region of the
metal shell/cup, and regions of obscuration can
be avoided. The inclination (relative to a tangent
line drawn between the inferior borders of the
ischial tuberosities) and the anteversion are
automatically calculated and tabulated. Both the
inclination and anteversion are corrected for the
effect of X-ray beam offset (7) (i.e. when the
beam is targetted in the region of the pubic
symphysis). The software has a facility to
discern whether the cup is in antversion or
retroversion. This requires two AP radiographs:
one standard pelvis radiograph and one hip
centred radiograph. These need to be taken in
succession so that the patient remains in the
same position.
The software has been validated using
radiographs of a laboratory model at different
settings (8).
1.
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR.
Dislocations after total hip replacement arthroplasties. J Bone Jt
Surg Am. 1978;60:217-220.1.
2.
Malik A, Maheshwari A, Dorr LD. Impingement with total hip
replacement. J Bone Jt Surg Am. 2007;89-A:1832-1842.
3.
Langton DJ, Jameson SS, Joyce TJ, Webb J, Nargol AVF. The
effect of component size and orientation on the concentration of
metal ions after resurfacing arthroplasty of the hip. J Bone Jt Surg
Br. 2008;90-B:1143-1151.
4.
Hart AJ, Skinner JA, Henckel J, Sampson B, Gordon F. Insufficient
acetabular version increases blood metal ion levels after Metal-on-
metal Hip Resurfacing. Clin Orthop Relat Res. 2011;469:2590-
2597.
5.
Wynn Jones H, Macnair R, Wimhurst J, et al. Silent tissue
pathology is common with a modern metal-on-metal hip
arthroplasty. Acta Orthop. 2011;82:301-307.
6.
Murray DW. The definition and measurement of acetabular
orientation. J Bone Jt Surg Br. 1993;75-B:228-232.
7.
Derbyshire B. Correction of acetabular cup orientation
measurements for X-ray beam offset. Med Eng Phys.
2008;30:1119-1126.
8.
Derbyshire B, Diggle PJ, Ingham CJ, Macnair R, Wimhurst J,
Wynn Jones H. A new technique for radiographic measurement of
acetabular cup orientation. J Arthroplasty. 2014;29(2):369-372.


Contact: